Prebiotics, Probiotics, and Postbiotics Explained: The Gut Health Hierarchy and why Postbiotics Matter More Than You Think

Walk into any health food store, and you'll find hundreds of probiotic supplements making bold claims about gut health. But after 15 years as a board-certified gastroenterologist specializing in longevity medicine, I can tell you: most people are investing in the wrong part of the equation.
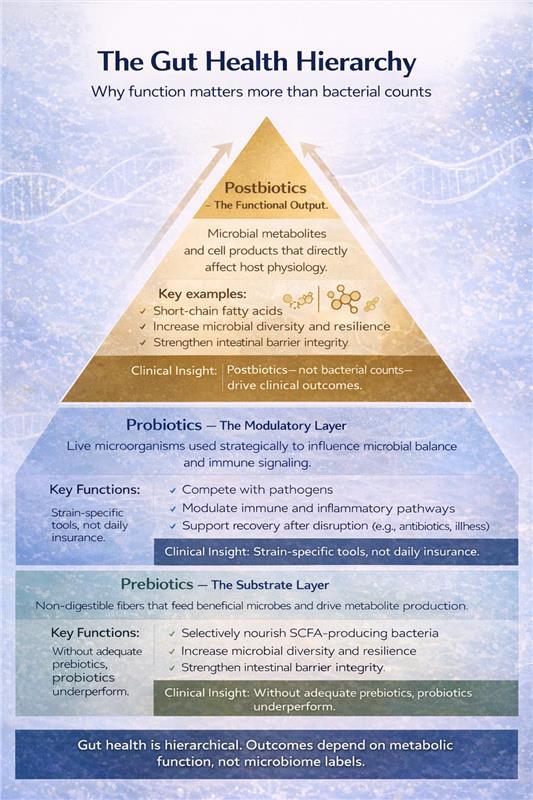
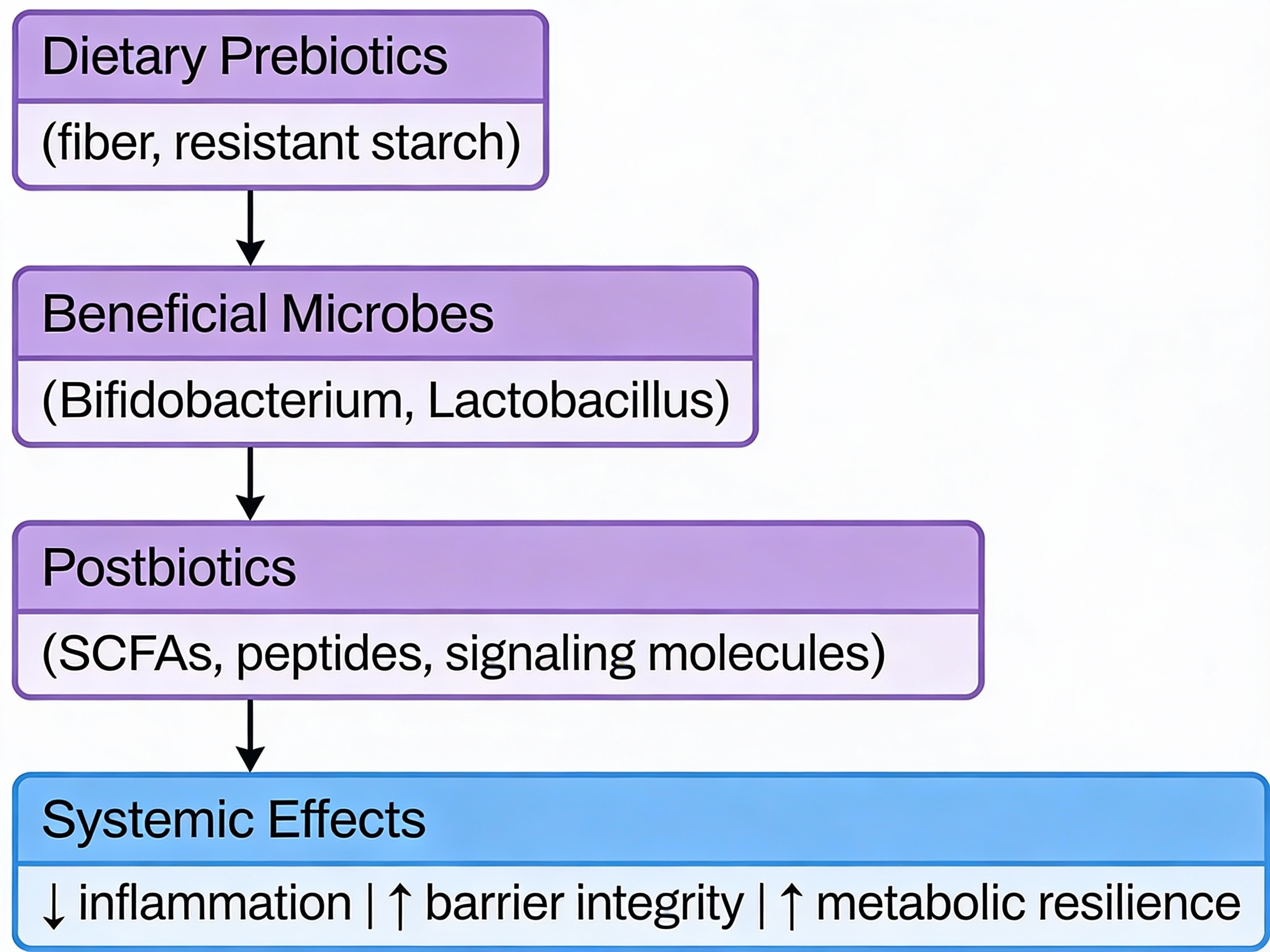
The real story of gut health isn't about adding more bacteria—it's about understanding how prebiotics, probiotics, and postbiotics work together, and why that matters for how you age.
Executive Summary
Prebiotics are specialized fibers that feed your beneficial gut bacteria.
Probiotics are live bacteria strains—useful in specific situations, not as daily insurance.
Postbiotics are the bioactive compounds your gut bacteria produce—these are what actually drive the health benefits.
Here's what matters for longevity: A healthy microbiome isn't about the number of bacteria you consume. It's about supporting the ones you have to produce the right metabolic compounds—particularly short-chain fatty acids like butyrate—that reduce inflammation, support metabolism, and influence the biology of aging itself.
Why Your Gut Microbiome Is a Longevity Lever
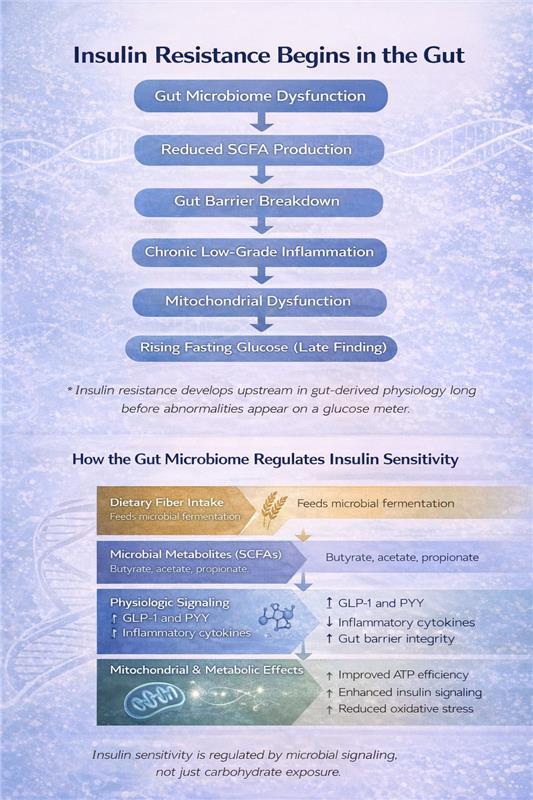
Your gut microbiome acts as a bridge between what you eat and how your body ages. It influences inflammation, insulin sensitivity, immune function, and even cognitive performance. As we age, microbial diversity typically declines, contributing to chronic inflammation, metabolic dysfunction, and frailty.
The good news? Your microbiome is one of the most modifiable factors in longevity medicine.
The Hierarchy: How I Approach Gut Health in My Clinic
1. Foundation: Prebiotics
Prebiotics are non-digestible fibers that pass through your small intestine intact and reach your colon, where beneficial bacteria ferment them. This fermentation produces short-chain fatty acids (SCFAs)—particularly butyrate—which strengthen your intestinal barrier, reduce systemic inflammation, and support metabolic health.
Key prebiotic types:
- Inulin (chicory root, onions, garlic, leeks, asparagus)
- Resistant starch (green bananas, cooked-and-cooled potatoes/rice, oats)
- Fructooligosaccharides (FOS) and galactooligosaccharides (GOS)
Practical implementation:
- Target 25-35g total fiber daily, including 5-10g prebiotic fiber
- Start low (5g) and increase gradually over 2-3 weeks to minimize gas/bloating
- Diversity matters—rotate different prebiotic sources throughout the week
- Cooked-and-cooled starches are often better tolerated than raw inulin sources initially
Clinical insight: In my practice, consistent prebiotic intake produces more durable microbiome improvements than probiotic supplementation alone. One patient with metabolic syndrome improved her HbA1c by 0.8 points over six months primarily through dietary fiber optimization and polyphenol-rich foods—no probiotics needed.
2. Targeted Tool: Probiotics
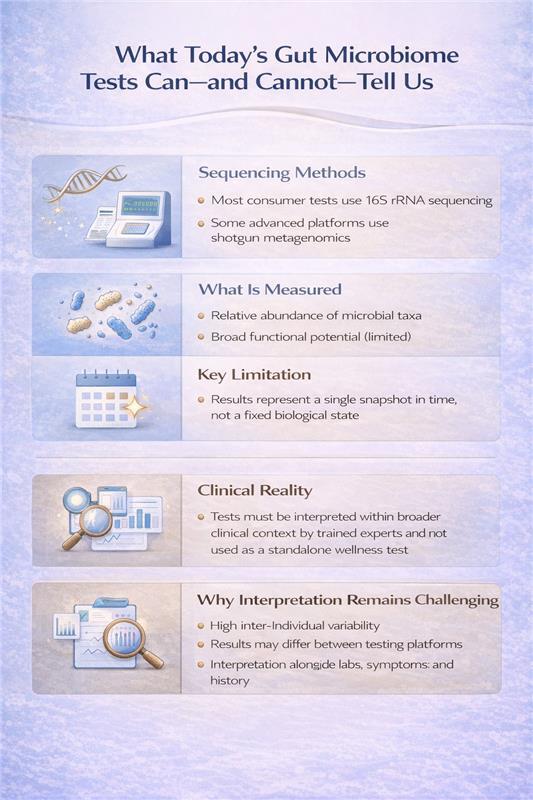
Probiotics are live microorganisms that confer health benefits when given in adequate amounts. But here's the critical distinction: probiotics are strain-specific clinical tools, not universal daily supplements.
When I recommend probiotics:
- During or after antibiotic courses (particularly Saccharomyces boulardii or Lactobacillus rhamnosus GG)
- Acute infectious gastroenteritis
- Specific IBS presentations (based on symptom pattern and strain evidence)
- Confirmed dysbiosis with targeted intervention goals
What to look for in quality probiotics:
- Genus, species, and strain clearly listed (e.g., Lactobacillus rhamnosus GG, not just "Lactobacillus")
- CFU count appropriate for indication (typically 1-10 billion)
- Third-party testing for viability
- Enteric coating or acid-resistant capsules for gastric survival
Reality check: Most healthy individuals don't need daily probiotic supplementation. Your microbiome is remarkably stable and self-sustaining when properly nourished. If you're reaching for probiotics as "microbiome insurance" without a specific indication, redirect that investment toward prebiotic-rich foods.
Caution: If you're immunocompromised or have central lines/prosthetic heart valves, discuss probiotic use with your physician first. While generally safe, live bacteria supplementation requires consideration in these contexts.
3. The Real Target: Postbiotics
Here's where it gets interesting. Postbiotics are the metabolic byproducts and cellular components produced by your gut bacteria—and they're what actually deliver the biological benefits we care about.
Key postbiotics include:
- Short-chain fatty acids (butyrate, acetate, propionate)
- Bacteriocins (antimicrobial peptides)
- Exopolysaccharides
- Certain vitamins and enzymes
- Microbial cell wall components
Why postbiotics matter for longevity: These compounds directly interact with your cells to modulate inflammation, support mitochondrial function, strengthen gut barrier integrity, and influence immune tolerance. Butyrate, for example, serves as the primary fuel source for colonocytes while also acting as a histone deacetylase inhibitor—influencing gene expression related to inflammation and aging.
The practical reality: While postbiotic supplements are emerging commercially, the most effective approach is supporting your microbiome's natural postbiotic production through prebiotic fiber, polyphenols, and microbial diversity. When I measure success, I'm looking at inflammatory markers (hs-CRP), metabolic parameters (fasting insulin, HbA1c), and clinical outcomes—not just microbiome composition.
Clinical advantage: Because postbiotics don't rely on live organisms, they're inherently more stable and appropriate for medically complex or immunocompromised patients. As this field matures, targeted postbiotic interventions may become a cornerstone of longevity medicine.
Prebiotics in the Diet: Practical Food Sources
A diverse intake across these foods supports microbial diversity and sustained postbiotic production.
Putting It Together: A Real-World Protocol
When a patient comes to me wanting to optimize their gut health for longevity, here's my typical approach:
Phase 1: Foundation (Weeks 1-4)
- Dietary assessment and fiber optimization (gradually increasing to 30-35g daily)
- Add diverse prebiotic sources: onions, garlic, asparagus, oats, legumes, cooked-and-cooled starches
- Incorporate polyphenol-rich foods: berries, green tea, extra virgin olive oil, dark chocolate
- Eliminate ultra-processed foods, excess added sugars, and artificial sweeteners
Phase 2: Assessment (Weeks 4-8)
- Monitor for improved regularity, reduced bloating, stable energy
- If significant GI symptoms persist consider comprehensive stool analysis
- Check inflammatory markers (hs-CRP) and metabolic parameters (fasting insulin, lipids)
Phase 3: Targeted Intervention (If Needed)
- Probiotics added only for specific indications: recent antibiotic use, confirmed dysbiosis, symptom-specific IBS treatment
- Duration: typically, 4-12 weeks, not indefinitely
- Reassess and discontinue if no clear benefit
Maintenance:
- Sustainable, fiber-rich dietary pattern (Mediterranean-style is my default)
- Ongoing prebiotic diversity
- Periodic reassessment of inflammatory and metabolic markers
When to Seek Professional Help
Consider working with a gastroenterologist or functional medicine practitioner if you experience:
- Persistent GI symptoms despite dietary optimization (bloating, pain, irregular bowel movements)
- History of recurrent infections or significant antibiotic exposure
- Autoimmune conditions or chronic inflammatory states
- Metabolic syndrome, insulin resistance, or unexplained weight changes
- Cognitive symptoms potentially linked to gut-brain axis dysfunction
The Longevity Perspective
The microbiome research is evolving rapidly, but the fundamentals remain clear: sustainable gut health comes from supporting microbial function and metabolic output, not from indiscriminately adding bacteria.
Think of it this way: prebiotics provide the fuel, probiotics can offer targeted support when needed, and postbiotics deliver the biological effects that influence how you age. The most powerful intervention is usually the simplest; nourishing the ecosystem you already have.
In my clinic, microbiome optimization follows a clear hierarchy:
- Diet-first, fiber- and polyphenol-rich nutrition
- Personalized prebiotic support
- Precision probiotic use when indicated
- Outcome-driven assessment focused on inflammation, metabolism, and resilience
Key Takeaways
- Prebiotics (fiber) are your foundation—they feed beneficial bacteria and drive SCFA production
- Probiotics are targeted tools for specific clinical situations, not daily insurance
- Postbiotics are where the real longevity benefits occur—support their natural production through diet
- Focus on microbial function and metabolic output, not just adding more bacteria
- A whole-food, fiber-rich diet consistently outperforms supplementation alone
Dr. Banerjee is a board-certified gastroenterologist with over 15 years of clinical experience, peer-reviewed publications indexed in PubMed, and deep expertise in gut microbiome science. He advises high-achieving individuals and families on precision longevity and healthspan optimization. Expanded clinical analysis is available through the Private Longevity Briefing.
Selected References
- Slavin J. Fiber and prebiotics: mechanisms and health benefits. Nutrients. 2013;5(4):1417–1435. doi:10.3390/nu5041417.
- Yalçıntaş YM, Bolino MJ, Duman H, et al. Prebiotics: types, selectivity and utilization by gut microbes. Int J Food Sci Nutr. 2025;1–27. doi:10.1080/09637486.2025.2582557.
- Riddle MS, DuPont HL, Connor BA. ACG clinical guideline: acute diarrheal infections in adults. Am J Gastroenterol. 2016;111(5):602–622. doi:10.1038/ajg.2016.126.
- Smolinska S, Popescu FD, Zemelka-Wiacek M. Pre-, pro-, syn- and postbiotics and intestinal integrity. J Clin Med. 2025;14(11):3673. doi:10.3390/jcm14113673.
- Aroniadis OC, Grinspan AM. The gut microbiome: a primer for the clinician. **Am J Gastroenterol.**2024;119(S1):S2–S6. doi:10.14309/ajg.0000000000002583.
- Fontana L, Bermudez-Brito M, Plaza-Diaz J, et al. Sources and evaluation of probiotics. **Br J Nutr.**2013;109(S2):S35–S50. doi:10.1017/S0007114512004011.
- Rana A, Smriti. Probiotics: mechanisms of action and GI health. J Sci Food Agric. 2025. doi:10.1002/jsfa.70275.
- Żółkiewicz J, Marzec A, Ruszczyński M, Feleszko W. Postbiotics—beyond pre- and probiotics. **Nutrients.**2020;12(8):2189. doi:10.3390/nu12082189.
- Thorakkattu P, Khanashyam AC, Shah K, et al. Postbiotics in food and pharmaceuticals. Foods. 2022;11(19):3094. doi:10.3390/foods11193094.
- Wegh CAM, Geerlings SY, Knol J, et al. Postbiotics in early life and beyond. Int J Mol Sci. 2019;20(19):4673. doi:10.3390/ijms20194673.
- Scott E, De Paepe K, Van de Wiele T. Health-modulatory postbiotic biomolecules. **Biomolecules.**2022;12(11):1640. doi:10.3390/biom12111640.
- Nataraj BH, Ali SA, Behare PV, Yadav H. Postbiotics and parabiotics. Microb Cell Fact. 2020;19:168. doi:10.1186/s12934-020-01426-w.
- Gurunathan S, Thangaraj P, Kim JH. Postbiotics as therapeutic agents. Foods. 2023;13(1):89. doi:10.3390/foods13010089.
- Cuevas-González PF, Liceaga AM, Aguilar-Toalá JE. Postbiotics: concepts to applications. **Food Res Int.**2020;136:109502. doi:10.1016/j.foodres.2020.109502.
- Amobonye A, Pillay B, Hlope F, et al. Postbiotics: latest advances. **World J Microbiol Biotechnol.**2025;41(8):293. doi:10.1007/s11274-025-04483-8.
.svg)